This article is a summary of recent studies done on the psychological burden and mental health issues emerging from the pandemic. It’ll be updated as and when new research provides more insights.
We’ve spent about a 100 days in fear and made dramatic changes to how we live. We are quarantined for weeks, scared of catching COVID-19, cities are in lock-down, we might lose our jobs, and we cannot see how this ends. Uncertainty about what the future holds, the isolation from loved ones, the restrictions on leisure, the disruption of old habits and routines, the newly developed fears and worries, etc. test our psychological health and resilience. Our well-being has been whammed, probably like never before. Because there is a rise in interest in coronavirus and mental health, I’ll highlight what we have learned from psychological studies conducted on the impact of the CoVID-19 pandemic.
The COVID-19 pandemic is not just a public health crisis for the duration of the disease, it is also a mental health crisis[1] and people’s psychological well-being needs to be addressed[2]. Calls to mental health hotlines have dramatically risen[3] for a variety of reasons like suicide ideation and addiction. Telehealth options like phone/chat/video counseling, self-help forums, mental health apps may be our only option in seeking professional help; and fortunately, these methods[4] are effective in dealing with stress, addictions, loneliness, fear, grief, anxiety, PTSD, suicide, and depression. A new form of therapy called structured letter therapy[5] (involves writing a document with questions and pointers) is already recommended as an alternative during quarantine. The mental health needs of healthcare workers and covid-19 patients should be a timely priority, and doctors argue[6] current efforts are not enough. One line of effort is the now-evidence-based[7] use of progressive muscular relaxation to alleviate anxiety and improve sleep in infected patients.
Let us first look at the results of a few survey studies done on the psychological impact and the mental health burden of the covid-19 pandemic.
A nation-wide survey[8] done on over 52,000 Chinese people measured psychological distress using the newly developed COVID-19 pretraumatic distress index (CPDI). It measures the frequency of anxiety, depression, specific phobias, cognitive change, avoidance and compulsive behavior, physical symptoms and loss of social functioning in the past week. About 29% had moderate psychological distress and 5% had severe psychological distress. Researchers found that women were more distressed on average than men and previous research[9] suggests that women are more vulnerable to stress with a higher risk of developing PTSD. People between 18 and 30 years of age as well as those above 60 years had the highest CPDI score indicating the most distress. These groups are vulnerable to mental health issues. The 18-30 age group is most exposed to information via social media, and they need to make educated risk-related decisions to run a house. The older population’s psychological distress is most likely tied to a higher mortality rate. Higher education was also linked to higher distress, possibly through increased self-awareness about health and detailed parsing of covid-19 information. Migrant workers also had moderate to severe distress scores which are partly explained by their concern with virus exposure during transport, delays in work, and anticipated loss of income. The survey also exposed a potential protective factor in coping with distress – available medical resources, efficient regional public health systems, and quality preventive and control measures. These factors explain why psychological distress reduced over time. They also reveal that distress is closely tied to the stress-inducing events such as official reports of community transmission.
Another survey[10] on 4607 Chinese highlights another psychological protective factor – self-control, and a vulnerability – perceived severity of COVID-19. They found that increased self-control reduces the risk of mental health issues but perceiving an exaggerated severity of the disease increases the risk of mental health issues. Moreover, self-control moderates the relationship between perceived severity and poor mental health. That means – self-control and self-regulation during the pandemic is not only beneficial for improving mental health for the average person, it is even more beneficial for those who are very scared of the severity of the disease.
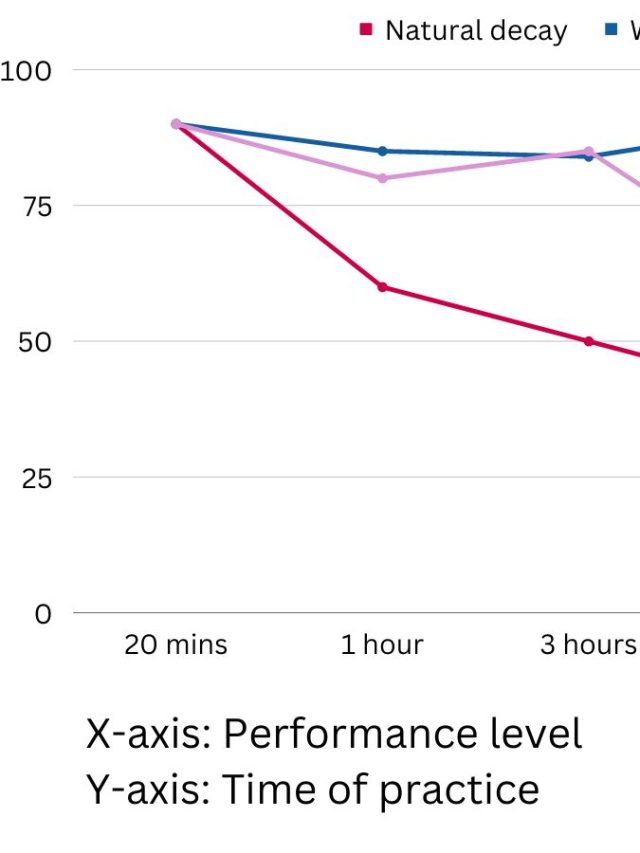
One small survey[11] (preprint, 603 volunteers) shows that the prevalence of generalized anxiety disorder was 34%, depressive symptoms was 18%, and poor quality sleep was 18%. Healthcare workers had the lowest quality of sleep. Exposure to covid-19 information/circumstances (over 3 hours) was associated with the highest anxiety. Healthcare workers (working 16-20 hours a day) and people consuming covid-19 content had the highest risk of deteriorating mental health. Yet another survey[12] on 1200+ Chinese people report higher numbers for psychological distress – 54% find the psychological impact of the pandemic moderate or severe. 16.5% reported moderate to severe depressive symptoms; 28.8% reported anxiety symptoms; 8.1% reported moderate to severe stress symptoms during the early phase of the epidemic in China. These numbers are higher in other reports[13] (preprint) which estimate the prevalence of depression, anxiety, and depression+anxiety to be 48%, 22%, and 19%. The report also highlights that social media exposure is positively correlated with increased anxiety – an insight corroborated by other studies as well.
Unsurprisingly[14], knowing people who are infected increases anxiety further. The same study found that social support is negatively correlated with anxiety which presses the now-well-known need for social support.
One of the hardest hit people are front-line healthcare workers who are not only in close contact with infected patients but also overworked and strained. In a survey[15] of 1563 medical staff, researchers found the prevalence of depression to be as high as 50.7%. Anxiety was as high as 44.7% and Insomnia was 36.1%. Other stress-related symptoms were present in 73.4% of the medical staff. During a relatively stable time, these numbers are closer to[16] 28% for medical students and 5% for professionals. During the SARS outbreak, healthcare workers were severely impacted and about 20%[17] had indicators of post-traumatic stress disorder.
Psychological issues and lifestyle considerations
A large team of behavioral scientists and psychologists highlight[18] some of the most pressing psychological issues in our response to the pandemic. I’ll highlight them here along with a few other insights from an earlier article I wrote on social distancing, mental health, and the pandemic.
1. Mindset: A healthy mindset impacts our approach to well-being. Believing that you are helpless or that stress is debilitating would worsen your well-being. But, on the other hand, approaching the pandemic as an “opportunity to improve personal skills” can enhance well-being. Mindsets about your own risk and body’s capacity to deal with it are likely to be very important in determining your well-being. Keeping a mindset like “we can manage this” is most likely to help. Over-exaggerating the pandemic by calling it a death sentence or underplaying it by calling it “just like the flu” can lead to maladaptive behavior, risk-taking, avoidance, denial, and negative emotions. Modifying your mindset to be constructive, realistic, and practical will help.
2. Interpersonal relationships: The lack of escape from people you live with or being forced to spend excessive time with someone may promote aggressive behaviors like shouting and abuse and increase conflict. Quarantines and social hang-out policies strain and drain psychological resources for empathy, patience, and tolerance. Even without a high-risk of infection, forced-time with someone can change a relationship’s dynamic, conversational content, and induce a wide range of negative emotions like anger, stress, and confusion.
3. Physical distancing: Social distancing causes loneliness for many and loneliness is an established risk for poor heart-health, low psychological well-being, mood disorders, and even suicide. One simple cognitive change is to call it physical distancing which removes a part of the emotional weight that social isolation and loneliness carries. The collective struggle to survive might bind us as a species, in spite of the loneliness and isolation.
4. Narcissism: Beliefs like “my nation is greater than others’ and has special characteristics” can be maladaptive. Nationalistic/Collective narcissism focuses on a nation’s identity instead of caring for it’s people – Caring for people is at the center of surviving the pandemic.
5. Social thinking: A thinking bias called ” the zero-sum-thinking” is especially relevant in decision making today and tomorrow. People tend to believe that someone else’s gain comes at the price of personal loss. However, the pandemic is a non-zero-sum event – other’s loss (infection) increases the likelihood of personal loss (community transmission). However, activities like hoarding are often zero-sum due to the limited amount of supply. Such a bias will affect us even after the curve flattens and the world regains a sense of normalcy – one person’s gain might help the society at large – the economy depends on people creating more and more value.
6. Conspiracy: Intellectual curiosity, a need for explanations, a compelling reason to blame someone, and exposure to various thoughts on the internet create a hotspot for conspiracy theories. Researchers expect a rise in conspiracy theories. Conspiring may stem from a perceived sense of spending time constructively and reducing uncertainty. People believe that large negative events require a proportionally large causal explanation. An intention-less microscopic biological machine such as the SARS-COV-2 virus may not be proportionally large enough to claim 50,000+ lives in a matter of weeks. Echo-chambers on the internet may reinforce and validate conspiracies. One defense against conspiracy theories is to inoculate people with small doses of facts and ask people to consciously judge the accuracy of content they share online. Conspiracy theories and misinformation satisfy frustrated psychological needs such as making sense, certainty, ascribing intention, affirming preconceived notions that are a part of one’s identity (racism, nationalistic pride, superiority complex). These reasons also promote a belief in pseudoscience.
7. Quarantine unhappiness: Tight rules during a quarantine or lock-down will reduce the rate of covid-19’s spread but it will also lower happiness and increase the risk for depression and suicide. These negative effects emerge from anxiety, lack of control, low social support, living in fear, perceived health risk, etc. Countries may need to choose a balance between strict lockdowns and a few loose constraints for the long-term well-being of whole communities.
8. Altruism: Disaster-time mindless panic is more of a pop-cultural myth than reality because studies show that a majority of people act altruistically, especially when[19] the positive effect of their altruistic/pro-social behavior and negative effect of selfish behavior is highlighted.
9. Strong emotions: People rely on their emotions to assess risks and take action. Stronger emotional reactions coming from anxiety and negative thoughts amplify the perceived risk of getting infected, even when countering numerical data exists (such as little to none cases nearby). Vulnerability perception[20] (risk perception) is often biased and many believe they have a lesser risk than others[21]. However[22], high anxiety increases perceived risk, especially when there is little control over the nature of the risk. Emotions also amplify in a social context[23] via “emotional contagion.” This is one of the reasons why it is extremely important to experience positive emotions and have meaningful engagement. Positive emotions and a good mood buffer against the impact of negative emotions.
The risk of anxiety, maladjustment, PTSD, depression, and other mental health issues has increased dramatically. Existing mental health issues can worsen and new ones can emerge. Share on X
Existential threats and prejudice against the Chinese
An existential threat is one of the biggest threats – it challenges our modest certainty of living our life as we know it. Existential threats range from an upheaval in society to complete disruption in an individual’s life; and in many cases, a question of life or death. A threat to our existence is a major source of anxiety, especially because anxiety is, by definition, our body and mind’s response to threat. We get anxious when something valuable about us – our mental health, physical safety, and psychological integrity is under attack (perceived & real). Fear of the unknown, especially fear of invisible agents like a virus, has social components. Public fear converts[24] into stigma, discrimination, and scapegoating (pointing fingers to play a blame-game) of specific people, scientists, and even public authorities.
One study[25] (preprint) done on 474 Americans (prior to the US declaring a national emergency) shows that Americans who believe that the coronavirus is a high-existential threat emerging from Wuhan, China develop a prejudice towards the Chinese people. People experience “anxious arousal” which promotes protective behaviors to protect oneself from the threat (social distancing, hoarding, panic buying) along with a prejudice toward the source of the threat. This is partly explained by people looking to blame someone/something for a threat and negatively evaluate the source of the threat. Such prejudice, if long-lasting can severely impact our social capital – the total “richness” of all relationships within a society. Blatant prejudice, as indicated by sentences like “I believe the Chinese are less able” (actual sentence in the study), will have long-term consequences. One way to overcome such prejudice is to believe that infected individuals are not directing a personal attack toward others, especially when there is asymptomatic transmission and others are behaving responsibly.
Psychological burden and Mental Health in Italy
One survey[26] on a nationally representative Italian population of 3,452 individuals has revealed insightful data. They collected the data between 18th March and 20th March – a time where Italy saw over 1500 coronavirus-related deaths. Here are the highlights.
- Over 90% (over 95% with a few exceptions) of all males and females across all age groups and self-evaluated health status strongly agree with and adhere to curfew norms and preventive measures like canceling social gatherings, washing hands, obeying curfew, and keeping 2m distance. Older people are more complaint than the younger ones. Those with self-reported poor health are less complaint in staying at home, possibly because of increased doctor and pharmacy visits.
- 78% believe that social distancing is an effective defense. 62% believe that the government’s response to the pandemic is appropriate and only 36% believe that other’s are reacting appropriately.
- Only 58% believe that the government has been truthful about information and 51% believe that the government will take care of them. Over 80% of skeptics hold pro-health beliefs and have a compliance score between 82% and 92%, except for the skeptics who also think the government and people are overreacting (score over 74%).
- 62% said they need to leave home in the next 5 days. The most common reasons they cited are buying food, visiting the pharmacy, going to work, walking a pet, and taking care of dependents. Only 18% cite non-essential reasons like breaking the law for the thrill, getting bored, meeting friends, etc. 18% refers to citing a reason, it may or may not be the only reason to go out as respondents chose multiple options in the survey to list reasons. Pharmacy visits were most common in older people and those with poor health, going to work was most common for middle-aged people, and walking a pet as well as exercise was most common for the younger ones.
- The most common negative aspects of staying at home are lack of freedom, boredom, lack of fresh air, loneliness, loss of job, lack of social activities. Different people and age groups highlight different negative aspects. Loneliness, family conflict, and boredom are the most common negative aspects for those with poor self-reported health. Middle-aged people are worried about the loss of a job. 18-29yo find boredom as the most negative aspect. Lack of exercise is the most common for those above 60+, possibly because of its medical benefits. Likely working parents consistently cite problems with homeschooling and economic distress as the worst aspects.
- The most common unsatisfied mental health needs are – freedom, stimulation, fresh air, exercise, social activities, income-source/work, and companionship.
- Almost everyone is moderately or severely anxious. The average anxiety score is 73.9 (on a 100 point scale). Those under 29 and those with self-reported excellent health are least anxious, but with a high anxiety score of 70. Females and those with poor health have the highest anxiety score (above 76).

Summary
The risk of anxiety, maladjustment, PTSD, depression, and other mental health issues has increased dramatically. Existing mental health issues can worsen and new ones can emerge.
Availability of public healthcare, medical resources, social support, and self-control are strong protective factors against declining mental health emerging from pandemic lockdowns and quarantines.
Exposure to information, thinking too much about information, high self-awareness about health, focusing on the severity of the disease make us vulnerable to mental health issues.
P.S. Most of the studies are correlational but with extensive survey and demographic data. Not all of them are peer-reviewed yet.
Sources
[2]: https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(20)30046-8/fulltext
[3]: https://www.indystar.com/story/news/health/2020/04/03/coronavirus-indiana-how-get-help-mental-health-addiction/5104357002/
[4]: https://www.liebertpub.com/doi/full/10.1089/tmj.2020.0068
[5]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7047000/
[6]: https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(20)30073-0/fulltext
[7]: https://www.sciencedirect.com/science/article/pii/S1744388120302784
[8]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7061893/
[9]: https://www.ncbi.nlm.nih.gov/pubmed/23408506/
[10]: https://psyarxiv.com/2xadq/
[11]: https://www.medrxiv.org/content/medrxiv/early/2020/02/23/2020.02.19.20025395.full.pdf
[12]: https://www.mdpi.com/1660-4601/17/5/1729
[13]: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3541120
[14]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7102633/
[15]: https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(20)30077-8/fulltext
[16]: https://www.sciencedirect.com/science/article/abs/pii/S0883944109001348
[17]: https://academic.oup.com/occmed/article/54/3/190/1390874
[18]: https://psyarxiv.com/y38m9/
[19]: https://www.nature.com/articles/s41562-018-0372-x.epdf?author_access_token=_jedfeEI4k6Y-H2WWZpF6tRgN0jAjWel9jnR3ZoTv0ONU7ol8kCn-T9ZzCi8dQtnDmdAOri1RdBXEnWoWCY6zH-VjWn7C8z71iSgvTvMH8ufgwrxznUQGyrLMWJYV3RtwoHbcO6NMC1C9Z8TtJM_XQ%3D%3D
[20]: https://link.springer.com/article/10.1007/s12529-008-9008-2
[21]: https://www.ncbi.nlm.nih.gov/pubmed/6536498?dopt=Abstract
[22]: https://www.tandfonline.com/doi/abs/10.1080/136698700376626
[23]: https://www.tandfonline.com/doi/abs/10.1111/j.1533-8525.2003.tb00532.x
[24]: http://211.103.242.144:1010/dzfw/yhjy/xgzl/202002/P020200210748043850573.pdf
[25]: https://psyarxiv.com/mpbtr/
[26]: http://expilab.com/wp-content/uploads/2020/03/covid-italy.pdf

Hey! Thank you for reading; hope you enjoyed the article. I run Cognition Today to capture some of the most fascinating mechanisms that guide our lives. My content here is referenced and featured in NY Times, Forbes, CNET, and Entrepreneur, and many other books & research papers.
I’m am a psychology SME consultant in EdTech with a focus on AI cognition and Behavioral Engineering. I’m affiliated to myelin, an EdTech company in India as well.
I’ve studied at NIMHANS Bangalore (positive psychology), Savitribai Phule Pune University (clinical psychology), Fergusson College (BA psych), and affiliated with IIM Ahmedabad (marketing psychology). I’m currently studying Korean at Seoul National University.
I’m based in Pune, India but living in Seoul, S. Korea. Love Sci-fi, horror media; Love rock, metal, synthwave, and K-pop music; can’t whistle; can play 2 guitars at a time.











Being mindful of the impacts that COVID-19 is having on mental health is key. Thanks for this!